Are you waking up with back pain and wondering, “can sleep apnea cause back pain?” Surprisingly, these two health issues might be connected.
Sleep apnea, known for disrupting sleep through breathing difficulties, may also play a role in back pain due to systemic inflammation and increased stress on the body.
This article delves into the possible links between sleep apnea and back pain to help you understand and address these interconnected health challenges.
Key Takeaways
-
Sleep apnea and chronic back pain are closely linked; poor sleep quality can exacerbate back pain due to increased inflammation and reduced effectiveness of natural opioids, while sleep apnea can lead to systemic inflammation, impacting the spine and contributing to conditions like disc degeneration.
-
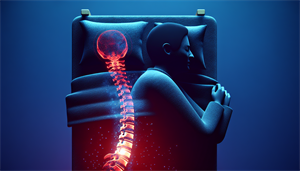
Poor sleep, such as that experienced by individuals with sleep apnea, can negatively impact spinal health by hampering the spine’s natural decompression and rehydration processes, and by straining the spinal column.
-
Treating sleep apnea may indirectly alleviate chronic back pain by reducing systemic and local inflammation and improving sleep quality, suggesting a need for an integrative treatment approach for patients suffering from both conditions.
Exploring the Relationship Between Sleep Apnea and Chronic Back Pain
Sleep apnea and chronic back pain, two conditions independently notorious for their debilitating impacts, are more interconnected than one might initially assume. Studies have found that sleep disturbances, such as those caused by sleep apnea, are frequently linked to low back pain. Poor sleep quality can intensify chronic back and neck pain, heightening inflammation and reducing the effectiveness of natural opioids, thereby amplifying pain and making it more challenging to alleviate.
Sleep apnea, particularly when left untreated, has a substantial impact on systemic inflammation in the body. The recurrent cycles of hypoxia (low oxygen levels) and reoxygenation, characteristic of sleep apnea, can lead to oxidative stress, thereby exacerbating inflammation. This inflammation can impact the spine, contributing to conditions like disc degeneration, which can result in persistent back pain. Hence, treating sleep apnea, including central sleep apnea, in conjunction with managing back pain is essential due to their interconnectedness. A comprehensive approach that considers this connection can result in more effective treatment outcomes compared to addressing each condition separately.
The Impact of Restless Nights on Spinal Health
Restless nights stemming from sleep apnea and restless leg syndrome can have a detrimental effect on spinal health, leading to exacerbated back pain and making it challenging to achieve a good night’s sleep. Inadequate sleep quality has been linked to spinal health problems, including chronic low back pain, waking spinal symptoms, and poor spinal alignment.
Maintaining spinal health depends heavily on sleep, as it facilitates the spine’s natural decompression process, rehydration of discs, and restoration of their optimal height. Poor sleeping posture can strain the spinal column, leading to the flattening of the natural curve. Additionally, poor sleep quality can trigger:
-
Migraine headaches
-
Back pain
-
Neck pain
-
Shoulder pain
-
Fatigue
-
Poor concentration
It is important to prioritize good sleep habits and ensure that you are using a supportive mattress and pillow to maintain proper spinal alignment during a good night’s sleep.
Thus, the quality of sleep directly influences the health of our spine, reaffirming the interconnectedness of sleep apnea and back pain.
How Oxygen Deprivation Affects Muscular Tension
Sleep apnea often results in oxygen deprivation due to frequent and prolonged interruptions in breathing. This leads to a decrease in oxygen levels in the bloodstream, which ultimately disrupts sleep patterns. Under severe hypoxic conditions, we can experience:
-
Muscle atrophy
-
Decrease in skeletal muscle cell number
-
Elevated muscle fatigue
-
Worsening of inactivity-related muscle wasting
-
Metabolic adjustments
-
Reduction of mass in skeletal muscle.
This muscular tension during oxygen deprivation can be attributed to metabolic adaptations and the loss of skeletal muscle mass. The insufficient generation of ATP due to suppressed oxidative phosphorylation is a significant contributor to this tension. Moreover, diminishing oxygen levels can have a notable impact on the maximal force output in skeletal muscles, affecting how back pain is experienced.
Thus, sleep apnea-induced oxygen deprivation can escalate muscular tension, a factor contributing to back pain, potentially leading to spinal deformities and increased risk of vertebral fractures, both associated with back pain.
Unraveling the Cycle: Poor Sleep Quality and Back Discomfort
The interplay of poor sleep quality and back discomfort is not a simple linear equation but a cyclical relationship. Pro-inflammatory cytokines and wide dynamic range neurons play a significant role in this cycle. Pro-inflammatory cytokines are signaling molecules that stimulate inflammation in the body. They are linked to sleep disruptions, such as insomnia, and can heighten pain receptors, resulting in heightened pain sensitivity. Furthermore, sleep deprivation can result in an elevation of these pro-inflammatory cytokines, as the deprivation itself can induce a heightened production of these inflammatory signaling molecules.
Wide dynamic range neurons can contribute to the development and maintenance of back discomfort, perpetuating the cycle of poor sleep and pain when they are activated and sensitized by factors such as sleep deprivation. This vicious cycle, in which pain impairs sleep and poor sleep further exacerbates pain, results in a continuous loop of discomfort and sleep disturbance.
Identifying and tackling this cycle is key to managing both untreated sleep apnea and back pain.
The Role of Pro-Inflammatory Cytokines
Pro-inflammatory cytokines are responsible for initiating or amplifying inflammation and orchestrating the immune system’s reaction to combat infections and other potential hazards. In the context of sleep apnea, these cytokines play a significant role. Sleep apnea can lead to systemic and local inflammation, resulting in a pro-inflammatory state. This is linked to elevated levels of inflammatory markers like IL-6 and TNF-α.
Patients with sleep apnea exhibit increased levels of these pro-inflammatory cytokines, further illustrating the interconnectedness of sleep apnea and back pain.
Understanding Wide Dynamic Range Neurons
Wide dynamic range (WDR) neurons, found in both superficial and deep layers of the dorsal horn, are essential for processing pain signals as they can respond to a variety of stimuli. They play a significant role in encoding the intensity of pain by responding to both noxious and non-noxious stimuli, thus making them essential in the regulation of nociception – the sensory nervous system’s response to harmful stimuli.
Disrupted sleep patterns, such as sleep deprivation, sleep apnea, and rem sleep, can lead to elevated adenosine levels, which exert an inhibitory influence on wide dynamic range neurons, thereby affecting their capacity to process pain signals. Sleep apnea can impact the activity of these neurons through several mechanisms, including intermittent hypoxia, hypercapnia, and negative airway pressure, which can result in neuronal impairment and dysfunction. The impact of sleep duration on these disrupted sleep patterns is an important factor to consider as well.
Understanding the role of these neurons provides a deeper insight into the connection between sleep quality and pain perception.
Identifying Symptoms: When Sleep Disorders Meet Chronic Pain
Recognizing the symptoms of both sleep apnea and lumbar spine issues can be a critical step in identifying the intersection between sleep disorders and chronic pain. Indicators of lumbar spine issues leading to persistent back pain include:
-
Low back pain, potentially arising from spinal degeneration or injury, muscle or ligament strain, and scoliosis
-
Shooting or tingling pain, which may indicate lumbar disc disease
-
Pain that radiates to other parts of the body
The symptoms of sleep apnea and chronic back pain often intersect as the lack of restful sleep often reported in chronic spinal pain increases hyperalgesia. This means that poor sleep quality due to sleep apnea can worsen the chronic back pain experienced by individuals with low back or lower back pain. Sleep apnea can worsen the symptoms of chronic back pain by disrupting the quality of sleep, leading to increased production of inflammatory substances in the body that contribute to the perception of pain.
Conditions like lumbar spine disorders are specifically linked to poor quality sleep, which can contribute to or exacerbate lower back pain.
The Interplay Between Sleep Apnea and Lumbar Spine Issues
The relationship between sleep apnea and lumbar spine issues is a complex one. Not only can sleep apnea contribute to conditions like lumbar spondylosis and elevate the risk of vertebral fractures, which can negatively impact the lumbar spine, but lumbar spine issues can also result in inadequate alignment during sleep, leading to strain on muscles and ligaments. This strain can cause discomfort in the neck and lower back, potentially worsening symptoms of sleep apnea.
Typical symptoms commonly observed in both sleep apnea and lumbar spine issues include:
-
Episodes of not breathing during sleep
-
Awakenings with shortness of breath
-
Difficulty maintaining sleep
-
Back pain worsened by restless sleep
Recognizing these symptoms can help us better manage these overlapping conditions.
Treatment Synergies: Addressing Sleep Apnea and Back Pain Together

When it comes to treating sleep apnea and back pain, a comprehensive, synergistic approach can offer enhanced and enduring relief for patients, ultimately improving their overall health and well-being. A combination of the following strategies can significantly improve the symptoms of both these conditions:
-
Using CPAP machines
-
Implementing pain management strategies
-
Engaging in physical therapy
-
Regular exercise
Regular exercise, for instance, can contribute to the alleviation of symptoms associated with both sleep apnea, such as snoring, and lumbar issues, like lower back pain, thus leading to an improvement in patient health.
CPAP Machine and Pain Management Strategies
One of the most effective treatments for sleep apnea is the use of a CPAP (Continuous Positive Airway Pressure) machine. A CPAP machine functions by administering pressurized air through the airway using tubing and a mask, thereby enhancing the quality of sleep. Various categories of CPAP machines are tailored to accommodate the diverse requirements of individuals with sleep apnea, such as Continuous PAP (CPAP), auto-adjusting PAP (APAP), and bilevel PAP (BiPAP).
Enhanced sleep resulting from the use of a CPAP machine can indirectly contribute to the management of chronic back pain by alleviating symptoms related to sleep apnea, which are linked to poor sleep quality and consequently, heightened pain in individuals suffering from chronic low back pain.
Physical Therapy and Regular Exercise

Physical therapy and regular exercise are instrumental in enhancing sleep quality and quantity, improving cardiorespiratory fitness, and possibly reducing dependence on pain medications for those with sleep apnea and chronic back pain. Specific exercises that can effectively lessen back pain linked to sleep apnea include:
-
Tongue stretches
-
Tongue push-ups
-
Tongue wag
-
Spoon hold
-
Jaw stretch
-
Singing
-
Yoga poses such as cat pose, cow pose, and back-opening breathing exercises.
Techniques considered effective for the management of chronic back pain include:
-
Tai chi
-
Yoga
-
Massage
-
Spinal manipulation
-
Exercises focusing on strengthening trunk muscles and enhancing endurance
-
Manual therapy
-
Education
-
Behavioral approaches
Lifestyle Changes to Improve Sleep and Reduce Back Pain

Lifestyle choices significantly impact the management of sleep apnea and the alleviation of back pain. Adhering to a consistent sleep schedule can aid in managing these conditions by enabling the mind and body to adapt to a regular sleep cycle, thereby enhancing overall sleep quality. Optimal sleeping positions for alleviating back pain include lying flat on the back or sleeping on the side with a pillow between the knees.
Additionally, limiting alcohol and caffeine consumption is important, as alcohol can exacerbate airway obstruction in individuals with sleep apnea, and caffeine can induce alertness and interfere with sleep when consumed near bedtime, potentially aggravating back pain.
The Importance of Sleep Hygiene
Sleep hygiene, the practices and habits that nurture healthy sleep, plays a vital role in managing sleep apnea and reducing back pain. Good sleep hygiene helps establish healthy sleep habits, reduces sleep deprivation, and promotes relaxation before bedtime, thereby reducing discomfort during sleep and promoting better spinal alignment.
For individuals with sleep apnea, advised sleep hygiene practices involve:
-
Adhering to a consistent sleep schedule
-
Correctly utilizing a continuous positive airway pressure (CPAP) machine
-
Establishing a sleep-friendly environment
-
Abstaining from stimulants
-
Engaging in relaxation techniques before bedtime to enhance sleep quality and minimize the effects of sleep apnea on back pain.
Diagnostic Pathways: From Sleep Study to Lumbar Spine MRI
Diagnostic pathways are essential for comprehending the link between sleep apnea and back pain. Sleep studies, or polysomnography, are used to diagnose obstructive sleep apnea (OSA) by identifying apnea and hypopnea, which are characterized by a decrease in nasal airflow lasting more than 10 seconds that corresponds with either a 3% oxygen desaturation or an arousal. The procedure of a sleep study includes recording brain waves and other bodily functions during sleep to diagnose sleep disorders.
A lumbar spine MRI aids in the diagnosis of back pain by capturing images of soft tissues such as the intervertebral disks, the spinal cord, and surrounding muscles. These images can reveal abnormalities or issues that contribute to the pain. Identifying these diagnostic pathways can help aid in the treatment of sleep apnea and chronic back pain, leading to more effective patient outcomes.
Patient Stories: Overcoming Sleep Apnea and Back Pain
The journey of patients overcoming sleep apnea and back pain through comprehensive treatment plans is a testament to the effectiveness of the discussed strategies. While the timeframe for observing improvements in the treatment of these conditions can vary, many individuals experience noticeable relief within approximately 6 weeks.
Patients have reported significant benefits from physical therapy and regular exercise in reducing the severity of sleep apnea, improving sleep quality, strengthening spinal support muscles, enhancing flexibility, and lowering inflammation, which ultimately provides significant relief from chronic back pain. The use of CPAP machines has also shown to be an effective method for managing pain in individuals who have both sleep apnea and back pain. These stories highlight the potential for improved patient outcomes with the right treatment approach.
Future Directions in Research and Treatment
The outlook for research and treatment in sleep apnea and chronic back pain is optimistic. Prospective research trends and ongoing clinical trials by renowned institutions aim to evaluate the efficacy of different treatments such as positive airway pressure and surgery for sleep apnea, along with exploring the association between obstructive sleep apnea and lumbar spine health.
Innovative treatments, such as the Inspire Sleep Apnea Innovation and potential medication AD109, are currently in development, offering the potential to improve back pain in patients with sleep apnea. Advancements in pain management practices and technology have significantly enhanced both the diagnosis and management of chronic back pain.
These potential advancements and ongoing research signify the strides we are making towards improving patient outcomes in the realm of sleep apnea and chronic back pain.
Summary
In conclusion, the interconnectedness of sleep apnea and chronic back pain is a complex puzzle that we are only beginning to understand. By recognizing the cycle of poor sleep quality and back discomfort, identifying symptoms, implementing synergistic treatment strategies, making necessary lifestyle changes, and utilizing diagnostic pathways, we can manage these conditions more effectively. As we continue to explore future directions in research and treatment, we remain hopeful for more comprehensive and effective treatment options. After all, the key to unlocking relief from sleep apnea and chronic back pain may lie within our understanding of their intricate connection.
Frequently Asked Questions
Can sleep apnea cause body aches and pains?
Yes, sleep apnea can cause body aches and pains, and there may be a relationship between pain and sleep disorders such as sleep apnea. Specifically, individuals with sleep apnea are at increased risk for long-term pain.
Can sleep apnea cause sciatica?
Although there is no definitive evidence linking sleep apnea to sciatica, it is clear that the combination of sleep apnea and back or sciatica pain can significantly impact sleep quality.
What part of the body does sleep apnea affect?
Sleep apnea affects the heart, leading to an increase in pressure on the blood vessels and chambers of the heart, ultimately causing damage to the heart muscle.
Symptoms of sleep apnea?
Some symptoms of sleep apnea include: [include list of symptoms]
How are sleep apnea and chronic back pain related?
Sleep apnea and chronic back pain are related as poor sleep quality and oxygen deprivation from untreated sleep apnea can contribute to spinal health issues, potentially leading to persistent back pain. This is because systemic inflammation caused by untreated sleep apnea can impact the spine and contribute to conditions like disc degeneration.