Are your night sweats a sign of sleep apnea? This article cuts straight to the heart of the matter, exploring the link between sleep apnea and night sweats. It provides clear insights into why disrupted breathing during sleep can lead to a damp awakening and what you could do to find relief. Keep reading to equip yourself with knowledge that may transform your nights.
Key Takeaways
-
Sleep apnea, specifically Obstructive Sleep Apnea (OSA), can cause night sweats due to stress hormone release during breathing interruptions, affecting body temperature.
-
While night sweats alone may not indicate sleep apnea, they, along with symptoms like excessive daytime sleepiness, loud snoring, and interrupted breathing, can suggest the need for medical evaluation for OSA.
-
Effective management of sleep apnea through CPAP therapy and lifestyle changes, such as weight loss and exercise, can significantly reduce night sweats and improve overall sleep quality.
Exploring the Intersection of Sleep Apnea and Night Sweats

Sleep apnea, a sleep disorder characterized by repeated cessation of breathing during sleep, often contributes to the occurrence of excessive sweating at night. Indeed, around 30% of male patients with Obstructive Sleep Apnea (OSA) report night sweats, which can result in excessive daytime fatigue. This connection between sleep apnea and night sweats highlights the importance of being aware of various medical conditions and their potential symptoms.
This association comes from the release of stress hormones during sleep apnea events, leading to increased body temperature and, consequently, experiencing night sweats.
The Role of Obstructive Sleep Apnea in Nighttime Sweating
Obstructive Sleep Apnea (OSA), a type of sleep apnea, is particularly notorious for causing nighttime sweating. This disorder is characterized by:
-
the obstruction of airways during sleep
-
leading to repeated cessation of breathing throughout the night
-
these breathing interruptions, coupled with the body’s stress responses, contribute significantly to night sweats.
Stress Hormones and Their Impact on Body Temperature

During an apnea episode, stress hormones are released, potentially elevating the body’s temperature. This increase in temperature can result in sweating, hence the connection between sleep apnea and night sweats. This process is triggered by frequent arousals during the night, which are caused by interruptions in breathing, affecting melatonin secretion due to exposure to abnormal nocturnal light and untreated conditions leading to increased blood sugar and fat levels as well as elevated blood pressure.
Unveiling Symptoms: When Night Sweats Signal a Deeper Issue
Night sweats can be a tell-tale sign of underlying health issues, such as sleep apnea. Should you manifest symptoms of sleep apnea and night sweats, it becomes necessary to seek medical advice and investigate suitable treatment options without delay.
While night sweats alone do not confirm a diagnosis of sleep apnea, the presence of other symptoms can provide a clearer picture of the condition.
The Symptom Spectrum of Obstructive Sleep Apnea
Obstructive Sleep Apnea (OSA) presents a range of symptoms, including:
-
Snoring
-
Choking
-
Headaches
-
Excessive dry mouth
Snoring, often associated with OSA, coupled with additional symptoms such as gasping or choking during sleep, could signal the presence of OSA or gastroesophageal reflux disease. These choking episodes result from the partial or complete blockage of the airway, leading to breathing pauses and a subsequent drop in oxygen levels in the blood, prompting the individual to wake up choking or gasping for air.
Headaches, another common symptom, may be attributed to oxygen desaturation leading to cerebral vasodilation. In individuals with OSA, the prevalence of sleep apnea headache is between 12%-18%.
Beyond the Sweat: Recognizing Other Indicators of OSA
Recognizing other indicators of OSA can help ascertain if night sweats are a result of sleep apnea or another underlying condition. The main indicators of OSA include:
-
Excessive daytime sleepiness
-
Loud snoring
-
Noisy and laborious breathing
-
Repeated short periods where breathing is interrupted by gasping or snorting.
Individuals with OSA frequently suffer from significant daytime fatigue and sleepiness due to inadequate restorative sleep during the night. Other symptoms include:
-
Waking up with a dry mouth or sore throat
-
Experiencing morning headaches, which increase in frequency and intensity with the severity of OSA
-
In children, OSA may also manifest as frequent nighttime urination and potential bed-wetting.
Diagnosing the Culprit: Sleep Studies and Sleep Apnea Detection
Diagnosing sleep apnea involves undergoing a sleep study, which can be conducted in a specialized sleep lab or even at the comfort of your own home. The sleep study helps to capture a comprehensive picture of your sleep patterns, thereby aiding in the diagnosis of sleep apnea.
Comprehending the Apnea-Hypopnea Index (AHI) is another crucial element in assessing the severity of sleep apnea.
Choosing the Right Sleep Study
Choosing between in-lab sleep studies and home sleep tests is a key decision in the process of diagnosing sleep apnea. In-lab sleep studies, also known as polysomnography, record multiple body systems, including brain waves, while a person sleeps in a lab setting.
On the other hand, home sleep tests offer the following benefits:
-
They monitor heart rate, oxygen levels, and breathing using small sensors at home.
-
They provide the convenience of a familiar and comfortable environment.
-
They are more cost-effective compared to in-lab sleep studies.
Understanding the Apnea-Hypopnea Index
The Apnea-Hypopnea Index (AHI), a crucial diagnostic tool, quantifies the frequency of apnea and hypopnea events per hour, thereby aiding in the assessment of the severity of sleep apnea. The AHI is determined by:
-
Summing the total count of apneas and hypopneas observed during a sleep study
-
Dividing it by the total duration of sleep
-
Resulting in an average number per hour.
The severity of sleep apnea is determined by the quantity of apneas and hypopneas identified during sleep, with specific thresholds established to categorize it as mild, moderate, or severe sleep apnea.
Treating the Duo: Reducing Night Sweats by Managing Sleep Apnea
Proper control of sleep apnea can alleviate night sweats and enhance sleep quality. The most effective non-invasive treatment for sleep apnea is Continuous Positive Airway Pressure (CPAP) therapy. This involves the use of a device that delivers pressurized air through a mask to keep the airway open during sleep, thereby preventing the collapse that causes sleep apnea.
In addition to CPAP therapy, lifestyle changes such as weight loss, avoiding alcohol and smoking, and regular exercise can also significantly improve sleep hygiene and reduce night sweats.
CPAP Therapy: A Breath of Fresh Air
CPAP therapy, the predominant non-invasive approach for treating OSA, can significantly alleviate night sweats. The therapy involves the use of a CPAP machine that delivers pressurized air through a mask or nosepiece, assisting with breathing during sleep. The continuous flow of air keeps the airway open, preventing interruptions in breathing that trigger apnea events and lead to night sweats.
Research has shown that the use of CPAP therapy can significantly decrease the occurrence of night sweats in patients with OSA. For instance, one study showed a reduction from 33% to an average of just 11%. This suggests that managing sleep apnea with CPAP therapy can provide significant relief from night sweats and improve the quality of sleep.
Lifestyle Adjustments for Better Sleep Hygiene
In addition to CPAP therapy, certain lifestyle changes can also help manage sleep apnea and reduce night sweats. Weight loss, for instance, has been found to be a highly effective treatment for managing sleep apnea. Even a moderate weight reduction or losing just 10% of body weight can result in substantial improvements in sleep apnea symptoms and severity.
Other lifestyle adjustments that can complement CPAP therapy include the use of special pillows and oral appliances. Special pillows, such as wedge pillows or positional pillows, can help manage sleep apnea by elevating the head, leading to improved breathing, reduced apnea events, and maintenance of an open airway during sleep. Meanwhile, oral appliances, which are custom-fitted, can help maintain an open, unobstructed airway in the throat during sleep.
Risk Factors and Prevention Strategies
Targeting risk factors and adopting prevention strategies can significantly contribute to controlling sleep apnea and night sweats. Some lifestyle factors that can influence the development and severity of these conditions include:
-
Obesity
-
Smoking
-
Consumption of alcohol
-
Consumption of caffeine
Engaging in regular exercise and adopting a healthy diet can contribute to weight management and hormonal balance, thereby preventing sleep apnea and night sweats.
Addressing Contributing Health Problems
Tackling health problems that contribute to sleep apnea and night sweats is a central component of prevention and management strategy. Hormonal imbalances, particularly those during menopause, can play a role in the occurrence of night sweats. Furthermore, menopause can diminish the protective influence of estrogen against sleep apnea, thereby elevating the risk of experiencing sleep apnea.
Addressing these underlying health issues, managing infections, and considering hormone therapy if necessary can help manage hormonal imbalances and prevent sleep apnea and night sweats.
Monitoring Menopausal Hot Flashes
For women in menopause, keeping track of and controlling hot flashes is a significant tactic to lessen night sweats and enhance sleep quality. Hot flashes can lead to night sweating and a decrease in estrogen levels, both of which contribute to night sweats. Moreover, menopause-related night sweats can significantly disrupt sleep, leading to discomfort and sleep disorders such as insomnia.
Effective approaches for monitoring menopausal hot flashes include:
-
Hormone therapy
-
Acupuncture
-
Hypnosis
-
Mindfulness meditation
-
Yoga
These strategies can help manage hormonal fluctuations during menopause, thereby reducing night sweats and improving sleep quality.
Navigating the Emotional Toll of Night Sweats
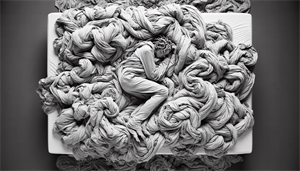
Persistent night sweats can heavily impact emotional health, causing feelings of anxiety, dread, and fear. The disruption of sleep and the associated discomfort can also cause emotional distress and impact mental health.
Support from family or support groups can play a vital role in managing the emotional impact of night sweats and improving overall well-being. It’s also important to visit primary care physicians for professional advice and guidance.
Summary
In conclusion, sleep apnea and night sweats are intricately linked. By understanding the role of Obstructive Sleep Apnea and stress hormones in causing night sweats, recognizing associated symptoms, and seeking a timely diagnosis, one can effectively manage these conditions. CPAP therapy and lifestyle changes offer promising strategies to reduce night sweats and improve sleep quality. Addressing risk factors and implementing preventive strategies are crucial steps towards managing sleep apnea and night sweats. Lastly, understanding and navigating the emotional toll of night sweats is essential for mental health and overall well-being.
Frequently Asked Questions
Can sleep apnea cause night sweating?
Yes, sleep apnea can cause night sweats due to the obstruction of necessary airflow during sleep, leading to symptoms such as choking and excessive dry mouth.
Why am I suddenly having night sweats every night?
It's important to see a doctor if you're experiencing frequent night sweats, as they could be due to underlying health issues like medication side effects, infections, or hormone changes. Don't hesitate to seek medical advice.
What are the warning signs of sleep apnea?
Common warning signs of sleep apnea include loud snoring, gasping for air during sleep, morning headaches, and excessive daytime sleepiness. It's important to be aware of these symptoms and seek medical attention if you experience them.
How can sleep apnea be diagnosed?
To diagnose sleep apnea, a sleep study is conducted either in a specialized sleep lab or at home, and the Apnea-Hypopnea Index is used to assess its severity.
What are some effective strategies for managing sleep apnea and reducing night sweats?
Using CPAP therapy is the most effective non-invasive treatment for sleep apnea and can greatly reduce night sweats. Additionally, adopting lifestyle changes like weight loss, avoiding alcohol and smoking, and regular exercise can also significantly improve sleep quality and reduce night sweats.


