Sleep apnea is a sleep disorder that affects millions of individuals globally, disrupting their sleep and potentially leading to other health complications. Recognizing the symptoms, understanding the causes, and exploring effective sleep apnea treatment strategies is crucial for managing this condition..
Key Takeaways
-
Sleep apnea is a common sleep disorder characterized by recurrent interruptions in breathing during sleep, caused by two primary types of disorders.
-
Professional guidance and personalized treatment plans are essential for managing sleep apnea effectively.
-
Home remedies such as abstaining from alcohol consumption, participating in regular physical activity, utilizing nasal strips and humidifiers can supplement professional treatments.
Understanding Sleep Apnea: Symptoms, Causes, and Types

Sleep apnea is a common sleep disorder characterized by recurrent interruptions in breathing during sleep. It’s akin to trying to drive with constant stop signs blocking your path – disruptive and frustrating. The condition can be classified into two primary types of sleep disorders – obstructive sleep apnea and central sleep apnea. These interruptions in breathing can lead to symptoms such as daytime sleepiness, disturbed sleep, and even high blood pressure.
While both types disrupt the sleep cycle, they differ in their causes. Obstructive sleep apnea is the more prevalent type, occurring when throat muscles relax, leading to airway blockage. On the other hand, central sleep apnea arises from inadequate brain signals to the breathing-controlling muscles. Comprehending these variations plays a pivotal role in the effective diagnosis and treatment of sleep apnea.
Obstructive Sleep Apnea
Imagine a busy highway, blocked by a sudden road closure - that’s what happens in mild obstructive sleep apnea. The throat muscles, acting as the roadblock, relax and cause a blockage in the airway, disrupting your sleep cycle. The evaluation process for treating this condition involves a comprehensive assessment, including a detailed medical history and a thorough physical examination that encompasses an evaluation of the throat, mouth, and nose.
Simple lifestyle changes can prove beneficial in managing this condition. For instance, individuals may consider sleeping on their side or stomach instead of on their back to prevent the throat muscles from obstructing the airway.
Advanced treatment options encompass upper airway stimulation, which involves a device that stimulates the forward movement of the tongue during inhalation, and a split-night sleep study that may entail the initiation of CPAP therapy if obstructive sleep apnea is diagnosed in the first half of the night.
Central Sleep Apnea
Like a conductor who orchestrates an ensemble, our brain is instrumental in regulating our respiration. In central sleep apnea, the brain fails to send proper signals to the muscles that control breathing. This type of sleep apnea is characterized by:
-
severe fatigue
-
daytime drowsiness
-
irritability
-
difficulty concentrating
-
frequent awakenings
These interruptions in breathing can lead to reduced oxygen levels in the body and potentially exacerbate underlying medical conditions such as heart failure and stroke.
For central sleep apnea, treatment options include:
-
Adjusting current medications
-
Using respiratory-stimulating drugs or hypnotics
-
Considering surgical interventions such as the implantation of a nerve stimulator
Though central sleep apnea is less prevalent compared to obstructive sleep apnea, it is as disruptive and needs to be addressed with equal attention.
The Role of Continuous Positive Airway Pressure (CPAP)

We now turn our attention to Continuous Positive Airway Pressure (CPAP), a prevalent and potent treatment for moderate-to-severe sleep apnea. Picture a guard at the palace gates, ensuring they remain open for the king’s entourage. In the same vein, CPAP provides a consistent flow of air through a mask to uphold an unobstructed airway during sleep, averting apnea occurrences. Using sleeping pills is not recommended for sleep apnea treatment, as they can worsen the condition.
In addition to CPAP, several types of positive airway pressure devices exist, including autotitrating positive airway pressure (APAP), bilevel positive airway pressure (BPAP), and adaptive servo-ventilation devices. These devices are designed to address diverse requirements and enhance the flow of air during sleep. The critical importance of CPAP in managing sleep apnea stems from its capacity to maintain an open airway and prevent breathing interruptions.
How CPAP Works
Examining the operation of a CPAP machine sheds light on its efficacy. The CPAP machine consists of a mask, a hose, and a machine with a fan that pulls air into the device. It’s akin to a gentle wind blowing continuously, ensuring the sails of a ship (your airways) stay open. The machine delivers a continuous flow of pressurized air that maintains the patency of the airways during sleep, mitigating any interruptions in breathing and diminishing apnea episodes effectively.
The standard pressure setting for a CPAP machine in sleep apnea treatment ranges from 4 cm H2O to 20 cm H2O. Think of it as the perfect wind speed, strong enough to keep the sails open but not too strong to capsize the ship. With the right settings and consistent use, CPAP can prove to be a game-changer in managing sleep apnea.
Challenges and Compliance
Despite its effectiveness, CPAP, like any therapy, brings its unique set of challenges. Comfort plays a significant role in adherence to CPAP treatment, with a substantial percentage of patients not adhering to the treatment due to discomfort. It’s like trying to sleep with a new pair of shoes on; it might feel odd and uncomfortable initially.
Users often express concerns regarding:
-
uncomfortable masks
-
leaky masks
-
excessive air pressure
-
feelings of claustrophobia
Psychological challenges like depression, anxiety, and sleep disturbances can also impact compliance with CPAP therapy. However, these challenges can be addressed with the help of a healthcare provider, ensuring that the CPAP treatment continues to effectively manage your sleep apnea.
Alternative Treatment Options for Sleep Apnea
Beyond the widely recognized efficacy of CPAP, it’s worth considering alternative treatment options. These include oral appliances, lifestyle changes, and surgical options. Like a toolbox filled with different tools, each treatment option serves a unique purpose and is selected based on the individual’s specific needs and condition.
There are several treatment options for treating sleep apnea, including treating obstructive sleep apnea with the following methods:
-
Oral appliances: These are specialized dental tools that work by advancing the lower jaw to open the airway during sleep.
-
Lifestyle modifications: This includes weight loss, increased physical activity, cessation of alcohol and tobacco use, and enhancement of sleep routines. These changes can help reduce the symptoms of sleep apnea.
-
Surgical procedures: In severe cases, or when other treatments have proven ineffective, surgical procedures may be considered.
Oral Appliances
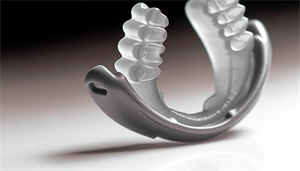
Oral appliances are like small, personalized tools engineered to modify the position of your jaw and tongue, sustaining an unobstructed airway during sleep. They come in various types, designed to address distinct requirements and enhance your comfort during sleep. The two main types are Mandibular Advancement Devices and Tongue Stabilizing Devices.
The journey to acquiring an oral appliance involves a series of steps:
-
Consultation with a physician or sleep specialist
-
Assessment of your condition
-
Tailoring the appliance for a suitable fit
-
Guidance on usage and maintenance
-
Regular follow-up appointments to confirm effectiveness
Lifestyle Changes

It’s often said, “A healthy outside starts from the inside,” and this rings true for managing sleep apnea. Lifestyle adjustments, such as refraining from excessive alcohol consumption and frequent use of sedatives, can help alleviate sleep apnea symptoms. Regular physical activities, including breathing exercises, tongue exercises, mouth and throat exercises, singing exercises, and yoga, can strengthen facial and throat muscles, enhance airflow, and minimize snoring.
In addition to these, maintaining a healthy weight plays a crucial role in managing sleep apnea. Weight loss can lead to a decrease in daytime sleepiness, an improvement in sleep apnea scores, and a reduction in the severity of this condition.
Surgical Options
For severe cases of sleep apnea, or when other treatments have proven ineffective, surgical interventions may be considered. Sleep apnea surgeries aim to diminish tissue in the posterior throat, advance the tongue, or implant a nerve stimulator to facilitate airway expansion, promoting improved breathing during sleep.
Popular surgical procedures include Uvulopalatopharyngoplasty (UPPP), which involves the removal of excess throat tissue, and nasal surgeries aimed at enhancing airflow through the nasal passages. The success rate of these surgeries varies, but they have demonstrated effectiveness in addressing sleep apnea. However, like any surgical intervention, they come with potential risks and side effects, such as excessive bleeding, infections, and additional breathing difficulties after the surgery.
Managing Sleep Apnea with Professional Guidance
Professional guidance is crucial in the diagnosis and management of sleep apnea. Regular appointments with a primary care doctor or an ENT specialist are essential for assessing the condition and making any required treatment modifications. Whether you’re struggling with the use of a CPAP machine or persisting sleep apnea symptoms, your healthcare provider can provide guidance and investigate the underlying causes of these issues.
Managing sleep apnea is a journey consisting of key steps such as diagnostic sleep studies, devising a personalized treatment plan, and maintenance of the treatment devices, like an oral appliance or a CPAP machine. Let’s delve deeper into these steps.
Sleep Studies and Diagnosis
Sleep studies are akin to a deep dive into your sleep pattern, providing insights into your sleep quality and identifying disruptions. The primary types of sleep studies used for diagnosing sleep apnea include:
-
Polysomnography (PSG)
-
Home Sleep Apnea Test (HSAT)
-
Electroencephalogram (EEG)
-
Electromyogram (EMG)
These studies meticulously record various body functions such as brain waves, oxygen levels, and breathing patterns to help diagnose sleep apnea.
Diagnosing the types of sleep apnea involves using polysomnography. In the case of obstructive sleep apnea, polysomnography detects instances of apnea, sudden awakenings with dyspnea, and challenges in maintaining sleep. To diagnose central sleep apnea, polysomnography reveals five or more central apneas and/or central hypopneas per hour of sleep. After the sleep study, it typically takes a few days to a couple of weeks for a sleep physician to evaluate and review the results.
Creating a Personalized Treatment Plan
After diagnosis, the journey to managing sleep apnea continues with the creation of a personalized treatment plan. The severity of sleep apnea is determined using the Apnea-Hypopnea Index (AHI), which measures the frequency of apneas and hypopneas during sleep. A higher AHI indicates a more severe case of sleep apnea, guiding the treatment strategy.
The personalized treatment plan should be regularly reviewed and updated to ensure the best possible outcomes. The frequency of these reviews and updates may differ based on individual circumstances and the recommendations of healthcare providers. Professional guidance ensures that the treatment plan remains effective and aligns with your evolving needs and condition.
Home Remedies and Self-Care Tips for Sleep Apnea
Although professional treatments are pivotal in managing sleep apnea, home remedies and self-care tips can supplement the treatment. From adjusting sleep positions to participating in regular physical activity, these simple changes can make a world of difference. It’s like adding a secret ingredient to a recipe; these changes can enhance the effectiveness of your treatment plan.
Home remedies that could offer temporary relief from mild sleep apnea symptoms include:
-
Adjusting sleep positions
-
Abstaining from alcohol consumption
-
Participating in regular physical activity
-
Addressing nasal congestion
-
Utilizing a humidifier to enhance nighttime breathing
It’s important to note that while these home remedies can provide temporary relief, they should not replace professional treatment.
Maintaining a Healthy Weight

Weight management is a crucial factor in handling sleep apnea. Excessive weight is a risk factor for sleep apnea, with a mutual relationship existing between weight and sleep apnea. Weight gain can exacerbate sleep apnea, and conversely, sleep apnea can contribute to weight gain. Therefore, maintaining a healthy weight is an important aspect of managing sleep apnea.
A reduction of only 10% of body weight can yield a substantial impact on sleep apnea symptoms. Think of it as getting rid of the extra luggage on a hot air balloon; losing weight can help alleviate sleep apnea symptoms and even lead to the resolution of sleep apnea in certain instances.
Nasal Strips and Other Home Remedies
Nasal strips are another helpful tool in your sleep apnea management toolbox. These strips function by expanding the nasal passages, facilitating enhanced airflow during sleep, potentially leading to a reduction in snoring. However, they do not tackle the root cause of the condition, and their effectiveness in managing sleep apnea symptoms is not substantial.
While nasal strips can provide temporary relief, it’s also important to address other factors such as alcohol consumption and physical inactivity. Abstaining from alcohol, participating in regular physical activity, and using a humidifier to enhance nighttime breathing can all contribute to managing sleep apnea symptoms.
Summary
Navigating the world of sleep apnea can be a complex journey, but with the right knowledge and guidance, managing this condition becomes a surmountable challenge. From understanding the types of sleep apnea and the role of CPAP to exploring alternative treatments and the importance of professional guidance, we’ve covered a vast landscape. Remember, whether it’s maintaining a healthy weight, using nasal strips, or getting regular check-ups, every little step contributes to managing sleep apnea effectively. Here’s to peaceful nights and energetic days ahead!
Frequently Asked Questions
What is the life expectancy of sleep apnea?
People with severe sleep apnea under 50 can expect to live between eight to 18 years if they receive treatment with oral appliance therapy or the CPAP machine.
Can sleep apnea go away?
No, sleep apnea is a chronic condition that cannot be entirely cured, but the symptoms can be treated with different forms of sleep apnea therapy and lifestyle changes.
Can I fix sleep apnea at home?
Yes, you can potentially manage obstructive sleep apnea at home through weight loss, lifestyle changes, and adjusting your sleep position. Obstructive sleep apnea occurs when the upper airway is partially or completely blocked.
What is the difference between obstructive sleep apnea and central sleep apnea?
The main difference between obstructive sleep apnea and central sleep apnea is that obstructive sleep apnea occurs due to relaxation of throat muscles, causing airway blockage, while central sleep apnea is caused by the brain not sending proper signals to the breathing muscles.
How does a CPAP machine work?
A CPAP machine works by delivering a continuous flow of pressurized air that helps keep the airways open during sleep, reducing breathing interruptions and minimizing apnea episodes. This can greatly improve the quality of sleep and overall health.


