Have you ever wondered about the symphony of sounds that echo in the night, the rumbles, snorts, and gasps that punctuate the silence? Far from being meaningless noise, these sounds could be signifiers of a common but often overlooked condition: sleep apnea. This blog post ventures into the nocturnal soundscape, distinguishing the harmless snores from the potentially concerning gasps, all in the quest to decode “what does sleep apnea sound like?”
Key Takeaways
-
Recognizing and comprehending the characteristic sounds associated with sleep apnea can help diagnose potential sleep disorders.
-
Bed partners can act as observers to detect signs of obstructive or central sleep apnea, while recording devices provide a detailed analysis of our sleeping patterns.
-
Treatments for Sleep Apnea vary depending on severity but typically include lifestyle changes such as weight management, exercise and changing sleeping positions.
Understanding Sleep Apnea Sounds

Sleep apnea, a disorder characterized by shallow breaths or pauses in breathing, is primarily treated to boost sleep quality. While many individuals with sleep apnea commonly exhibit symptoms like loud snoring and daytime sleepiness, they might not be aware of the more subtle signs. That’s where the power of sound comes into play. One can recognize the presence of this sleep disorder better by paying attention to its distinctive sounds such as chronic snoring, gasping for air, and interrupted breathing.
The nighttime symphony of someone with sleep apnea is often punctuated by a chorus of snores, gasps, and pauses. These sounds can act as warning signals, alerting us to potential sleep disorders. Recognizing and comprehending these sounds is the initial step towards improving sleep health.
Snoring and Sleep Apnea
Snoring is like the percussion section of our nocturnal orchestra, providing a steady rhythm to our nighttime soundscape. But not all snoring is the same. It’s the pattern and sound of the snoring that can hint at the presence of sleep apnea. The typical snoring associated with obstructive sleep apnea (OSA) is chronic, often accompanied by episodes of gasping for air during sleep, which are like unexpected cymbal crashes disrupting the rhythm.
Factors such as old age, obesity, enlarged tongues or tonsils, and specific head and neck shapes are risk factors associated with OSA. Acknowledging these factors, along with understanding how snoring can evolve into OSA, emphasizes the importance of awareness and medical evaluation for OSA.
So, the next time you dismiss snoring as just an annoying habit, remember, it could be the drumbeat of a deeper issue.
Gasping for Air

Gasping for air during sleep may be the equivalent of a startling trumpet blast in our nocturnal symphony. These gasps may result from various factors, including obstructive sleep apnea. The physiological process entails the narrowing or closure of the airway due to muscle relaxation in the throat, causing breathing interruptions and reduced oxygen intake, leading to daytime symptoms like excessive sleepiness.
In sleep apnea patients, particularly those with obstructive and central sleep apnea, gasping for air is a common symptom. So, while it can seem alarming, these sudden gasps could be a vital clue in our quest to decipher sleep apnea.
Pauses in Breathing
Imagine a symphony with sudden moments of silence, disrupting the melody. Pauses in breathing during sleep are much like these unexpected silences, breaking the rhythm and serving as a key indicator of sleep apnea. Apnea refers to the temporary cessation of breathing, particularly during sleep, with these events generally lasting approximately 10 to 30 seconds.
An individual with sleep apnea may experience these pauses in breathing anywhere between 120 and 239 times during an eight-hour sleep period. During these pauses, the individual experiences a cessation of breathing for a duration typically lasting 10 to 20 seconds. This can result in decreased oxygen levels, leading to symptoms such as snoring, gasping, and involuntary body movements upon awakening. These pauses or ‘moments of silence’ in our symphony could reveal vital information about our sleep health.
Types of Sleep Apnea and Their Unique Sounds
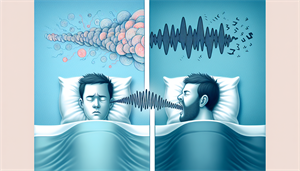
Just like a symphony can be divided into movements, each with its unique character, sleep apnea can be categorized into types, each with its distinctive sounds. The primary classifications of sleep apnea are obstructive sleep apnea (OSA) and central sleep apnea (CSA), with OSA being significantly more prevalent.
OSA is distinguished by pronounced snoring, choking, and gasping as the airway constricts and experiences repeated obstruction during sleep, resulting in decreased or halted breathing. On the other hand, CSA is characterized by more subtle breathing disruptions, such as shallow or irregular breathing and occasional gasping. Comprehending the distinctive sounds linked to each type of sleep apnea can aid in precise identification and diagnosis.
Obstructive Sleep Apnea Sounds
The sounds associated with Obstructive Sleep Apnea (OSA) are not unlike a tempestuous symphony movement. Loud snoring, often exceeding 53 dB(A), along with snorting, choking, and gasping are the usual auditory indicators of OSA. These sounds manifest when the airway experiences partial or complete blockage during sleep.
The distinctive snoring and gasping sounds in OSA are a result of the narrowing of the airway during sleep, leading to breathing disruptions. Despite being disruptive, these sounds act as essential indicators of a possible sleep disorder.
Central Sleep Apnea Sounds
Central Sleep Apnea (CSA) presents a stark contrast to the stormy sounds of OSA. It is characterized by irregular breathing during sleep and a lack of respiratory effort, often leading to silent pauses in breathing rather than loud snoring. These subtle disruptions in the nocturnal symphony can often go unnoticed but are equally significant.
The breathing disruptions in CSA are attributed to a breakdown in communication between the brain and the respiratory muscles, leading to irregular breathing patterns and intermittent pauses. Identifying these minor alterations in our nighttime soundscape rhythm is key to diagnosing CSA.
Identifying Sleep Apnea in Yourself and Others
Decoding the nocturnal soundscape and identifying sleep apnea can often feel like trying to understand a complex piece of music. However, by listening carefully to the sounds of our sleep – the snores, gasps, and pauses – we can recognize the patterns indicative of sleep apnea. In this process, both self-observation and the observations of others can play a significant role.
A bed partner’s observations are vital for identifying sleep apnea as they can recognize symptoms such as:
-
loud snoring
-
gasping
-
choking sounds
-
breathing pauses
-
sleep-induced restless movements
These symptoms may go unnoticed by the individual. It’s not just about listening to the melody but understanding the rhythm and the patterns that can provide vital insights into our sleep health.
Bed Partner Observations
A bed partner can act as an insightful listener, observing and decoding the sounds of sleep. They are often the first to notice the signs of sleep apnea, from the rhythmic snoring punctuated by pauses, to the sudden gasps for air. In this nocturnal symphony, they play a crucial role, much like a conductor leading the orchestra, helping to identify the symptoms that may otherwise go unnoticed.
Snoring patterns that could potentially indicate the presence of sleep apnea include loud and persistent snoring, snoring that is interrupted by pauses in breathing, and snoring accompanied by gasping or choking sounds. These minor rhythm alterations and unexpected interruptions can offer critical clues regarding sleep apnea’s presence.
Recording Your Sleep
In the quest to understand our sleep sounds, technology can be a valuable ally. Sleep recording devices, ranging from wearables like:
-
Apple Watch
-
Garmin
-
Fitbit
-
Oura Ring
To more advanced medical devices such as polysomnography (PSG) devices, can provide a detailed analysis of our sleep patterns, as they use cookies and data to track and record information.
These devices monitor a variety of physiological data during sleep, including:
-
Breathing patterns
-
Awakenings
-
Oxygen levels
-
Muscle movement
By providing a detailed analysis of our sleep, these devices help us understand our sleep patterns better and detect any anomalies that could be indicative of sleep apnea.
Health Risks Associated with Sleep Apnea
Much like a discordant symphony can have a lasting impact on the listener, sleep apnea, if left untreated, can have severe health consequences. From cardiovascular complications to cognitive and emotional effects, the impact of sleep apnea extends far beyond the realm of sleep.
Sleep apnea, especially when obstructive sleep apnea (OSA) is untreated, can significantly impact cardiovascular health. It can potentially lead to conditions such as:
-
high blood pressure
-
heart failure
-
stroke
-
type 2 diabetes
This is due to diminished oxygen levels during sleep. In addition to these risks, untreated sleep apnea can lead to persistent sleeping difficulties that can impact cognitive abilities and emotional health.
Cardiovascular Complications
The impact of sleep apnea on cardiovascular health is much like a discordant note disrupting the harmony of a symphony. OSA can put additional strain on the heart, leading to cardiovascular issues such as high blood pressure, heart disease, and stroke.
Increased cardiac effort to sustain blood circulation is a result of repeated airway obstructions during sleep. This can eventually lead to nocturnal hypertension and sustained high blood pressure during waking hours, which may cause morning headaches. Thus, the seemingly innocuous sounds of sleep could be the harbinger of serious health risks.
Cognitive and Emotional Effects
Sleep apnea’s cognitive and emotional effects can be likened to a complex symphony’s subtle undertones - frequently overlooked, yet significant. Sleep apnea can significantly impair cognitive functions, particularly affecting:
-
Concentration
-
Attention span
-
Executive functions
-
Memory
In today’s digital world, it is essential to protect against spam fraud and abuse in order to maintain the security and privacy of your online accounts and personal information.
Moreover, research has shown a clear connection between sleep apnea and depression. Studies have revealed that individuals with OSA have a higher likelihood of experiencing symptoms of depression and even developing major depressive disorder (MDD). Thus, the effects of sleep apnea extend beyond physical health, impacting mental and emotional wellbeing as well.
Diagnosing and Treating Sleep Apnea
Understanding the symphony of sleep sounds is just the beginning; decoding these sounds and using them to diagnose and treat sleep apnea is the next step. The diagnosis of sleep apnea involves a sleep study, or polysomnography, and is often conducted by a sleep specialist. Once diagnosed, the aim of treatment revolves around reducing breathing disruptions and enhancing sleep quality.
Treatment options for sleep apnea include:
-
Continuous Positive Airway Pressure (CPAP) therapy, which is often regarded as the ‘gold standard’ for treating sleep apnea
-
Oral appliances
-
Positional therapy
-
Lifestyle changes
Sleep Study for Diagnosis
A sleep study, or polysomnography, is like a detailed analysis of our nocturnal symphony. It involves observing a person’s breathing patterns during sleep, usually done overnight in a specialized lab or at home. This exhaustive study, which tracks a range of physiological data including:
-
breathing patterns
-
brain waves
-
heart rate
-
oxygen levels
is used to diagnose sleep apnea and assess its severity.
Polysomnography is widely acknowledged as the most dependable type of sleep study. It provides a detailed insight into our sleep patterns, helping us understand the rhythm of our sleep and recognize any disruptions that could be indicative of sleep apnea.
Treatment Options
Once diagnosed, sleep apnea can be effectively managed with various treatment options. CPAP therapy is a medical intervention that uses a device to deliver filtered and pressurized air through a mask into the airway during sleep. This process helps to keep the airway open, promoting regular breathing, stabilizing blood oxygen levels, and enhancing the overall quality of sleep.
Besides CPAP therapy, other treatment options entail oral appliances that keep the jaw or tongue in a specific position to prevent sleep-induced airway obstructions, and surgical procedures for those with physical airway obstructions or those requiring nerve stimulation for breathing regulation. The choice of treatment often depends on the severity of sleep apnea and the individual’s specific circumstances.
Preventative Measures and Lifestyle Changes
While understanding and treating sleep apnea is crucial, prevention plays an equally important role. Much like how a well-tuned instrument can create beautiful music, certain lifestyle adjustments can help prevent sleep apnea or alleviate its symptoms. These adjustments include:
-
Weight loss
-
Regular exercise
-
Quitting smoking and alcohol
-
Avoiding certain medications
-
Changing sleep positions
Weight management plays a significant role in managing sleep apnea. Maintaining a healthy weight can help prevent airway obstruction, and even a modest reduction of 10% in body weight can significantly diminish symptoms like excessive daytime sleepiness and irritability. Let’s delve deeper into these preventative measures.
Weight Management
Excessive weight, particularly in the neck region, can lead to breathing obstruction during sleep. However, weight management can help mitigate these risks. A mere 10% reduction in body weight can lead to an improvement in sleep apnea symptoms. Hence, the maintenance of a healthy weight through dietary measures and physical activity is pivotal in mitigating the risks associated with sleep apnea and alleviating its symptoms.
It’s like tuning an instrument – a little adjustment can make a big difference. Adopting a weight loss plan like the Mediterranean diet can aid in weight reduction and ease sleep apnea symptoms. The right diet, combined with regular exercise, can help you hit the right notes in your sleep health symphony.
Sleep Position and Environment
Just as a musician needs the right environment to create beautiful music, an optimal sleep environment can help minimize sleep apnea symptoms and promote better sleep quality. The most effective sleep positions for alleviating sleep apnea symptoms are sleeping on the side, especially on the left side, as these positions aid in keeping the airway open and decreasing the severity of apnea episodes.
Establishing an optimal sleep environment requires maintaining a dark, quiet, and cosy bedroom with a comfortable temperature. Environmental factors significantly influence the sleep quality of individuals with sleep apnea. High temperatures can lead to poorer sleep quality, exposure to bright light before bedtime can interfere with the ability to fall asleep, and noise can be a sleep disruptor.
So, whether it’s adjusting the sleep position or creating the perfect sleep environment, every change makes a difference in our nocturnal symphony.
Summary
In conclusion, the symphony of sleep is not merely a random arrangement of sounds but a complex melody with significant meaning. By understanding the unique sounds associated with sleep apnea, recognizing their significance, and acting upon this knowledge, we can better manage our sleep health. Whether it’s making lifestyle changes, seeking medical advice, or simply tuning into the sounds of our sleep, every step brings us closer to the ultimate goal – a harmonious, restful night’s sleep.
Frequently Asked Questions
What does someone with sleep apnea sound like sleeping?
Someone with sleep apnea may sound like they are snoring, snorting, or gasping while sleeping, indicating a potential obstruction in their upper airway. It is important to be aware of these signs as they may suggest the presence of sleep apnea.
What are 3 symptoms of sleep apnea?
The three common symptoms of sleep apnea include: loud snoring, pauses in breathing during sleep, and abrupt awakenings accompanied by shortness of breath. If you experience any of these symptoms, it's important to consult a healthcare professional for proper diagnosis and treatment.
What can be mistaken for sleep apnea?
Sleep apnea can be mistaken for conditions such as diabetes, GERD, low testosterone, hypothyroidism, sexual dysfunction, depression, and high blood pressure. It's important to consult a healthcare professional for accurate diagnosis and treatment.
How can I check if I have sleep apnea?
You can check if you have sleep apnea by undergoing a test called overnight sleep study (polysomnogram) in a medical facility, where you will be monitored while sleeping. This test monitors your heart, lung, and brain activity, breathing patterns, and blood oxygen levels.
How is sleep apnea diagnosed?
Sleep apnea is diagnosed through a sleep study conducted by a doctor or sleep specialist, which involves monitoring various body systems during sleep to observe breathing patterns, brain waves, heart rate, and oxygen levels.


